Reimagining primary care visits for people living with obesity
- owenhaskins
- Aug 26, 2025
- 3 min read
Researchers from Drexel University's College of Nursing and Health Professions, working with people living with obesity, have redesigned what an ‘ideal’ primary care visit could look like and validate their ideal visit concept among a sample of adults with obesity.
Navigating health care can be challenging under any circumstances, and systemic barriers can make the experience even more difficult for some groups. Weight-related stigma and inequities in health care can create barriers and negatively influence the experiences of people in larger bodies or living with obesity when visiting primary care physicians. These negative experiences can often lead to health care avoidance.
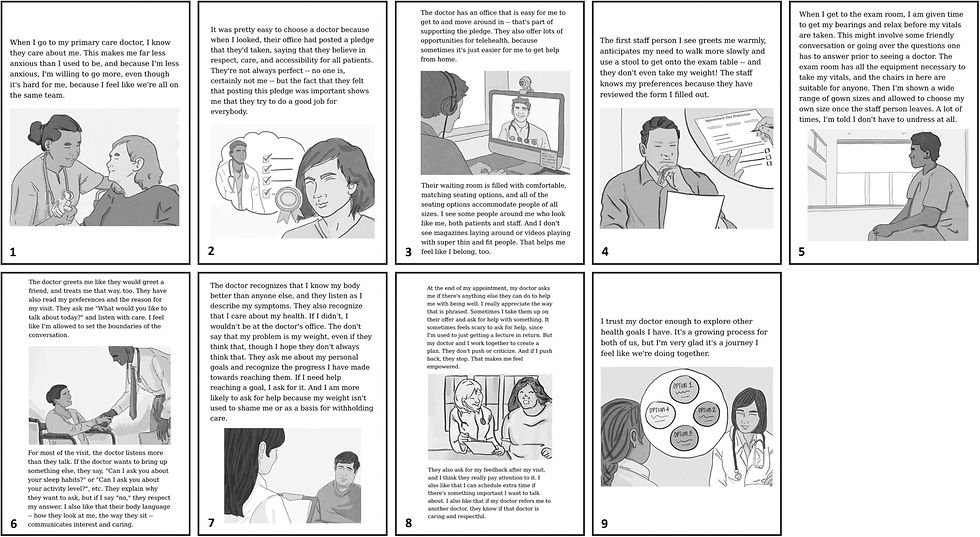
In the first phase of the study, the Obesity Action Coalition (OAC) and Thoughtform, an experience design studio, partnered with people living with obesity to create a story-based scenario showing a more ideal experience - one where patients feel listened to, treated kindly and not judged for their weight.
Participants shared experiences, challenges and solutions related to primary care, such as feeling a limited or lack of rapport with the clinicians or not having the physical space, being more welcoming by having different sizes of blood pressure cuffs and gowns available. Then OAC and Thoughtform, with the participant input, created an ideal primary care visit as a narrative scenario with illustrations.
In the second phase of the study, the research team surveyed 250 American adults with obesity to review this ideal scenario and compare it to their most recent real-life doctor visit. Most survey respondents preferred the ideal scenario, rating it an average of 9.4 out of 10. They especially liked it because it included things like doctors who listen attentively, showing respect and don't blame every health issue on weight. People also said it was important to be referred to specialists who treat them with respect and empathy.
"The survey results showed that people living with obesity want empathetic, respectful health care," said Dr Kristal Lyn Brown, an assistant professor in the College and lead author on the study. "We hope these results encourage providers and their staff to make their spaces more inclusive and free of weight bias and stigma."
Brown added that the findings underscore the importance of treating everybody as a human and not less than: "People with obesity are asking for basic, every day, human interactions - not resource-intensive changes but literally common-sense practices, of which our primary care offices often fall short."
The research team noted that by improving everyday interactions, people with obesity might feel more comfortable attending primary care visits, rather than avoiding them. Further, partnering, listening and being respectful could lead to increased trust between providers and patients living with obesity.
Considering the results of the study, the research team recommends that clinician training should explicitly address weight stigma and emphasize respectful, patient-centred communication. Further, the visit often starts with front office staff, which underscores the importance of ensuring all staff are equipped with the skills and awareness to recognise and address bias, ensuring every patient feels valued from the moment they arrive.
Referral practices should consider specialists that are also respectful and empathetic. Respectful, patient-centred communication would allow patients to tell their story before assuming their visit is related to their weight.
Lastly, Brown noted that this study highlights the importance of broader adoption of including patient voices in research to help with systems-level changes.
The findings were reported in the paper, 'Reimagining primary care visits for people living with obesity: A Co-design and validation study', published in Patient Education and Counseling. To access this paper, please click here





Comments