Tailoring the dose of botulinum toxin and refining the injection technique is safe and effective for patients living with obesity
- owenhaskins
- Jul 8, 2025
- 4 min read
Gastric botulinum therapy using a novel full-stomach injection method focusing on the antrum and fundus is safe and effective in Japanese patients living with obesity, according to a study by Dr Kodai Takahashi, a Bariatric Endoscopist and General Surgeon from Tokyo Takahashi Clinic Nerima, Tokyo, Japan.

“This study demonstrates that tailoring the dose of botulinum toxin and refining the injection technique according to individual patient characteristics are critical for enhancing both the efficacy and safety of gastric botulinum therapy,” the study authors stated. “This technique may offer a promising, minimally invasive option for obesity management. Future research is expected to further standardise these treatment techniques, ultimately promoting their broader clinical application.”
In some countries, gastric botulinum toxin therapy is gaining attention as a non-invasive treatment for obesity. However, existing studies show inconsistent results and a lack of standardised protocols around the type of botulinum toxin, injection sites and doses etc. Therefore, in this retrospective, single-centre study, Takahashi and colleagues evaluated the efficacy and safety of a novel whole-stomach injection method emphasising the antrum and fundus, as opposed to antral-only methods used in prior studies.
Eligible patients were defined as those with a BMI > 25 kg/m² who had obesity-related comorbidities and had failed to achieve weight loss despite prior dietary and exercise therapy.
Failure of dietary and exercise therapy was defined as less than 5% total body weight loss over a minimum of six months of supervised lifestyle intervention. Comorbidities such as diabetes mellitus, hypertension, and dyslipidaemia were diagnosed based on medical records and physician-confirmed diagnoses according to Japanese clinical guidelines.
The amount of botulinum toxin administered was adjusted according to the patient’s BMI. Specifically, patients with a BMI of ≥25 kg/m2 received 300 units (U) of Coretox, and those with a BMI of ≥30 kg/m2 received 400 U of Coretox. Botulinum toxin was reconstituted with 30 mL of preservative-free normal saline for the 300 U dose and 40 mL for the 400 U dose.
The following injection technique, originally developed by the authors for this study, was used to achieve uniform distribution of botulinum toxin throughout the stomach. First, 1 mL of botulinum toxin was injected in four quadrants at a point 2 cm proximal to the pyloric ring. Additional 1 mL injections were then performed in a systematic manner every 4 cm along the greater curvature, extending from the distal antrum to the gastric cardia. In total, injections were administered at approximately 30-40 sites, depending on individual gastric length.
This technique was specifically designed to ensure full stomach coverage, including the antrum, corpus, and fundus, with proportional dosing adjusted to gastric anatomy. The intent was to enhance the delay of gastric emptying and suppress ghrelin secretion by targeting both motility and hormonal axes. According to the authors, this whole-stomach injection method has not been previously described in the literature and represents a novel protocol devised in the context of clinical practice and anatomical optimisation.
Follow-up evaluations were conducted at approximately one month, three months and six months post treatment. Adverse events were actively monitored during scheduled follow-up visits and through interim phone interviews conducted by clinic staff. The primary outcome of this study was the percentage of total body weight loss (%TBWL) at six months following the procedure.
Outcomes
A total of 144 patients underwent whole-stomach botulinum toxin injection therapy with targeted emphasis on the antrum and fundus, between February 2023 and November 2024. The cohort comprised 82 females (56.9%) and 62 males, with a mean age of 41.7 ± 11.5 years and a mean baseline BMI of 31.4 ± 4.8 kg/m².
The procedure was technically successful in all cases and no intraoperative or delayed complications were reported. The mean procedure time was 5.7±1.2 minutes (range: 4.2-8.1 minutes), reflecting high procedural efficiency suitable for outpatient day-surgery settings.
The mean %TBWL at each time point (Figure 1) was as follows: one month: 6.5% ± 2.1% (interquartile range (IQR): 5.2-7.8%); three months: 10.2% ± 3.4% (IQR: 8.0-12.4%); six months: 12.2% ± 4.2% (IQR: 9.5-14.6%).
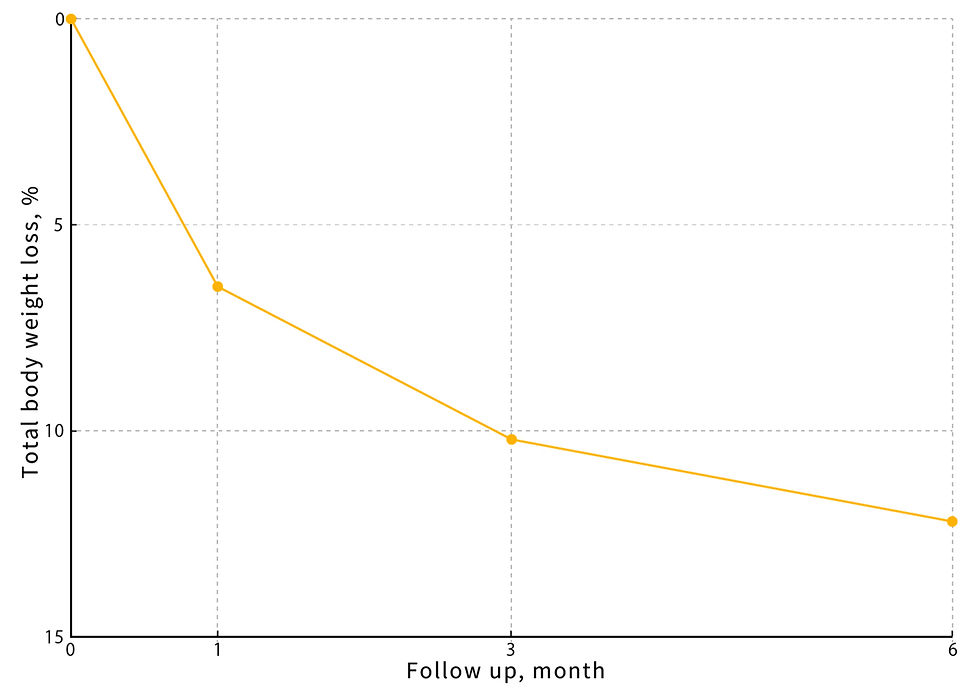
At six months, patients with a baseline BMI ≥35 kg/m² achieved a %TBWL of 13.8% ± 3.9% (IQR: 11.2-16.4%), compared to 11.1% ± 4.1% (IQR: 8.6-13.7%) in those with BMI <35 kg/m². Although this difference did not reach statistical significance (p=0.07), it may suggest a trend toward a BMI-dependent treatment response. Additionally, at the six-month follow-up, 78.5% (113/144) of patients achieved greater than 10% TBWL, a commonly used benchmark for clinically meaningful weight loss.
All 144 patients completed the treatment protocol, including scheduled follow-ups at one, three, and six months. No adverse events requiring clinical intervention were reported. Patients were monitored through in-person visits and telephone follow-ups at one, three, and six months post procedure. The assessment included symptoms such as nausea, abdominal pain, and signs of delayed gastric emptying. No hospitalisations or emergency interventions were required.
Treatment tolerability was assessed using a five-point Likert scale questionnaire administered at the one-week post-treatment follow-up. Although the questionnaire was not formally validated, it was developed based on clinical experience. Overall, 96.5% of patients rated their experience as either “excellent” or “good.”
“Ideally, it would be best to perform an endoscopy beforehand to determine gastric size and then decide the dose,” the authors noted. “However, many patients refused preoperative endoscopy, making this difficult to implement.”
Compared to prior studies employing antral-only or fundus-only botulinum injection, the whole-stomach approach in this study resulted in a higher %TBWL, suggesting a potential synergistic effect when both regions are targeted simultaneously. The authors hypothesise that this broader distribution may enhance the suppression of gastric motility and appetite-regulating hormones, particularly ghrelin, thereby improving weight loss outcomes. These findings support the notion that injection strategy, including anatomical targeting, plays a crucial role in therapeutic efficacy.
The findings were reported in the paper, ' Endoscopic Botulinum Therapy for Obesity: Focus on the Antrum and Fundus', published in Cureus.
To access this paper, please click here





Comments