Last patient receives Mizagliflozin in Phase 2 clinical study for the treatment of post-bariatric hypoglycaemia
- owenhaskins
- Apr 2, 2024
- 2 min read
Vogenx has completed dosing of the last patient in its Phase 2 clinical study VGX-001-012 evaluating Mizagliflozin in patients diagnosed with post-bariatric hypoglycaemia (PBH).

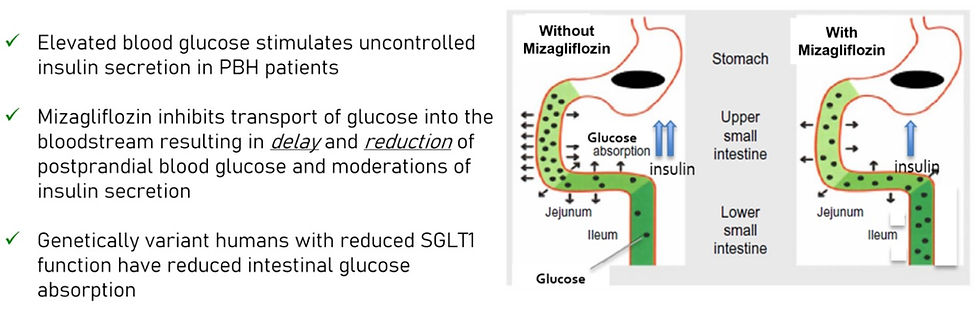
Mizagliflozin is an investigational first-in-class, oral, small molecule drug candidate that reduces postprandial glucose absorption and secretion of insulin and gastric inhibitory peptide (GIP). Through this mechanism, mizagliflozin has previously demonstrated statistically significant improvements in postprandial peak glucose and glucose nadir while reducing secretion of insulin and GIP, thereby reducing postprandial reactive hypoglycaemia in patients diagnosed with PBH. Mizagliflozin has been administered to over 500 subjects in clinical studies.
The multicentre, randomised, single-blind, placebo-controlled, dose-ranging and regimen-finding study enrolled 15 patients actively struggling with symptoms of PBH. Each patient was dosed with two doses of mizagliflozin and placebo, each for seven days (21-day study period) with a one-week washout period between regimens. Mixed meal tolerance tests were administered at the conclusion of each treatment period, and all patients wore blinded continuous glucose monitors throughout each treatment period.
"We are pleased to announce that we have dosed the last patient in our Phase 2 clinical trial evaluating mizagliflozin in patients with PBH," said James Green, Vogenx chief executive officer. "With no currently approved therapeutics, PBH is increasingly becoming a large, underserved market where patients are inadequately relieved of their symptoms. We are encouraged by what we continue to learn from our participating patients and believe that mizagliflozin has the potential to become an effective and well-tolerated therapeutic option for patients suffering from PBH."
PBH is an increasingly recognized chronic side effect of bariatric surgeries that are commonly performed as a treatment for obesity and related comorbidities. Neuroglycopenic symptoms can include shakiness, dizziness, confusion, sweating and loss of consciousness. These symptoms can be debilitating with a significant negative impact on quality of life, can dangerously impair normal day-to-day activities and can be life-threatening.
Bariatric surgery has proven to be the most effective treatment for severe obesity, leading to significant improvements in body mass index and obesity-related co-morbidities. It is estimated that over 9% of the US population has a body mass index above 40 which is considered severely obese. With over 250,000 bariatric surgery procedures performed per year in the United States, postoperative prevalence of hypoglycaemia symptoms in bariatric surgery patients is thought to be as high as 38.5%. There are currently no therapeutics approved by the FDA for the treatment of PBH.
The company expects topline data from this study to be available summer of 2024.




Comments